Is living intentionally the key to true happiness?
How often do we find ourselves drifting through life? Things may be fine but then suddenly we’ll feel stressed, anxious or angry as though out of the blue! Perhaps we’ve fallen into a life of […]
Read moreHow do we really embrace difference?
A hit single from the Disney film Pocahontas, Colours Of The Wind has the following verse: You think the only people who are people are the people who look and think like you. But if […]
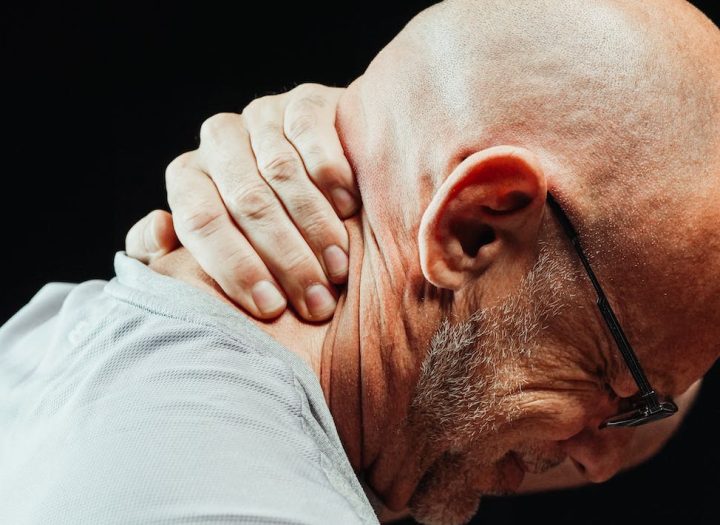
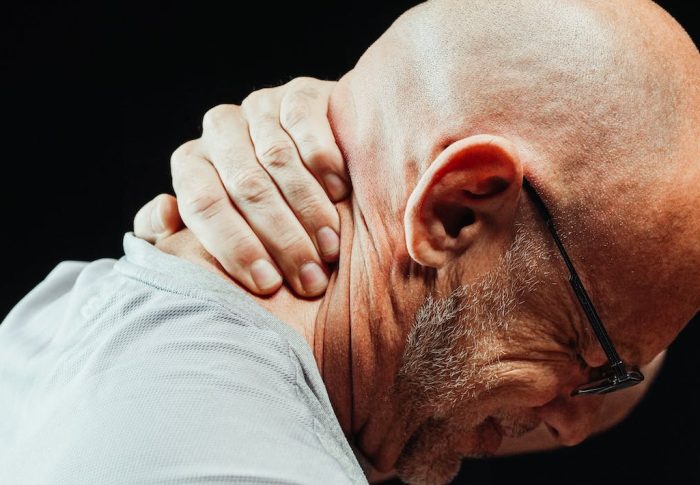
Read moreBeing honest about the true effects of chronic pain
Chronic pain conditions are complicated. Especially when you’re managing an additional insult such as a car accident. Taking care of ourselves is hard!
Read more